Person-Centred Care Planning 101
The care sector is experiencing a shift in the way practices and health systems are designed and managed. Traditionally, the role of patients and their families has been one of passive “order takers”. Nowadays, many service providers are implementing a person-centred approach. This requires a shift to viewing patients and their families as active “team members”.
Remind me again, what is a person-centred approach?
There is no single definition of person-centred (UK) or patient-centered (US) care. However, there are several elements commonly held across a variety of health settings:
- When coordinating care and desired outcomes, consider the well-being of the whole person (emotional, sexual, mental, physical, spiritual, cultural, socioeconomic status).
- Care and support plan with the person, taking into account their expressed interests, needs, preferences, and concerns. To this end, care is collaborative, empowering, and accessible.
- Systems and services orientate themselves toward enabling patients to recognize and build upon their strengths, rather than focusing on setbacks or incapabilities.

Brilliant. And why is this approach so important?
- Saves money and time: When people take an active role in managing and understanding their own healthcare, they choose less costly and invasive treatments, are less likely to use emergency services, and are more likely to stick to their treatment plan.
- Eases the burden on health care services: The earlier someone adopts healthy practices, the better chance they have of living at home longer and requiring fewer health interventions, reducing some of the pressure on health and social services.
- Motivates staff and patients: Practitioners feel confident and satisfied when able to deliver effective, compassionate care. Patients feel understood and empowered by their involvement in their own care. This boosts morale for both parties.
- Improves the quality of healthcare: Research has found that offering care in a more person-centred way tends to improve outcomes for patients and professionals.
Alright, so how do I make a care plan person-centred?
- Prepare: Identify what new roles and ways of working will be needed within your team. Someone must be responsible for preparing the process, holding discussions, coordinating appointments, and working closely with the practitioner or coordinator. There should be a plan for how to prepare and support the patient, ensure they are kept at the center of the process, complete necessary tests or assessments and have access to their information in a preferred way.
- Change the conversation: This is perhaps the biggest change when it comes to the shift from traditional to patient-centered care planning. Rather than giving indisputable advice, practitioners are expected to facilitate a coach-like conversation for shared-decision making. Explore what matters to the person, their priorities and outcomes, and ideas for moving towards these. The conversation should focus on supporting people in self-management of their health. Being grounded in the belief that people are the experts of their own lives, this requires a different way for practitioners to think about enabling thoughtful risk-taking and supporting people to discover ways to achieve their outcomes.
- Create the plan: Ideally, have one care and support plan. It may link to other plans and records as needed. Within an individual’s care plan there should be an overview with key points to know about a person, what is important to them and how they want to be supported. It should also explicitly link to any detailed plans a person may have for the future. However it is recorded needs to work for the individual, the practitioner and the organization.
- Review the plan: Give the review the same emphasis as the conversation. It provides a time to reflect on progress, revisit outcomes and plan how to move forwards. Information from patient-centered eviews informs the co-produced process, going on to inform service development and commissioning priorities.
That was a great summary, but I want more in-depth information for putting this into practice…
Personalised Care and Support Planning Handbook - NHS England
Patient Centered Care Improvement Guide - Institute for Healthcare Improvement
Personalised Care and Support Planning Tool - Coalition for Collaborative Care
Collaborative Care and Support Planning Toolkit - Royal College of General Practitioners
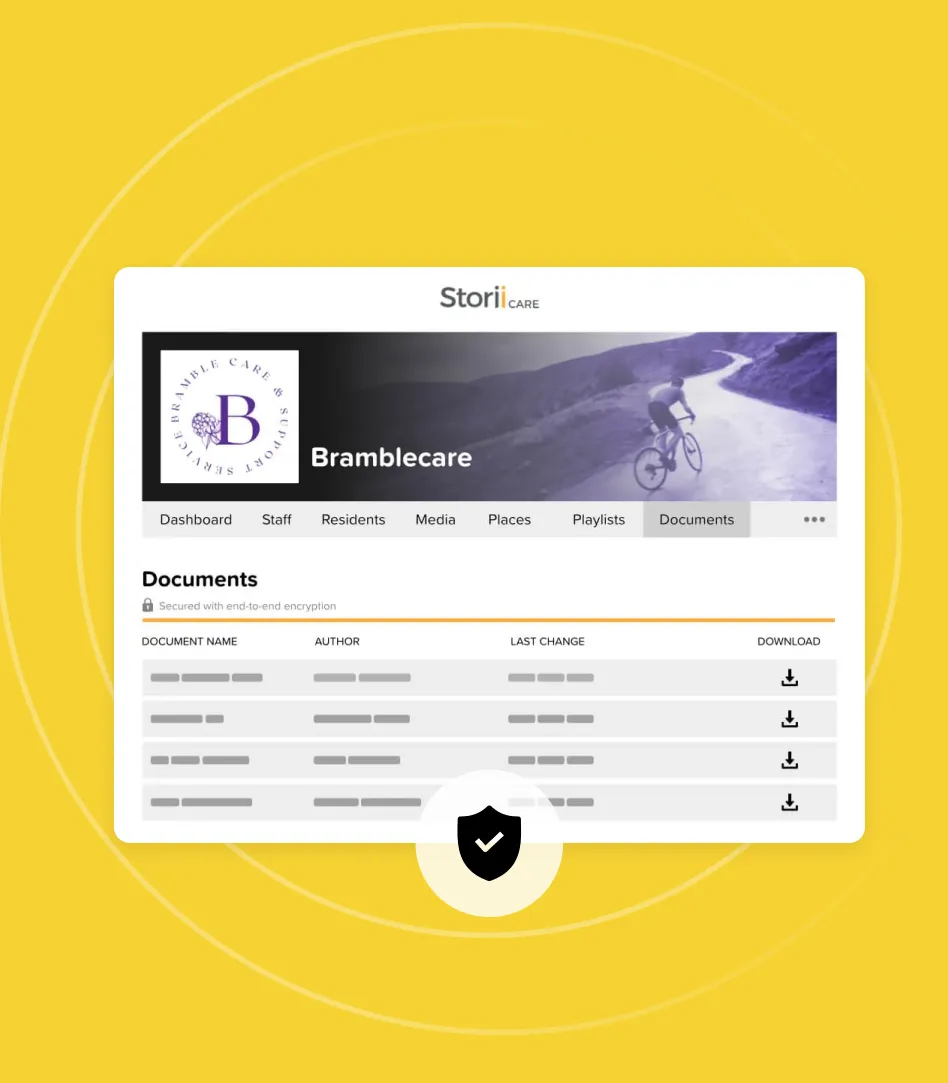
How StoriiCare Can Help
StoriiCare is a user-friendly care coordination and activities management software. With StoriiCare on your tablet or device, care staff can build up comprehensive, person-centred support plans with ease.
Interested? Click here to see how it works.




.png)
.png)
.png)